Antibiotic-associated diarrhea (AAD) is characterized by loose, watery stools three or more times a day after taking antibiotics used to treat bacterial infections. AAD can develop in 5–35% of patients taking antibiotics, depending on the type of drug, health condition, and contact with pathogens. Studies show that all groups of antibiotics can lead to AAD, but the highest risk is associated with broad-spectrum drugs such as cephalosporins, fluoroquinolones, penicillins, and clindamycin.
Risk Factors
AAD can develop in anyone taking antibiotics, but the risk increases under the following conditions:
- You have had antibiotic-associated diarrhea in the past.
- You are taking antibiotics for a prolonged period.
- You are taking more than one antibiotic.
- You are taking antibiotics in high doses.
- The antibiotic you are taking has a broad spectrum of action.
Even weak antibiotics with a narrow spectrum of action can cause changes in the gut microbiota. The risk of developing AAD is especially high during the eradication of Helicobacter pylori, when two antibiotics are used simultaneously and for an extended period of 14 days. In this situation, the risk of disrupting the microbiota balance significantly increases.
Fluoroquinolones can trigger diarrhea caused by the dangerous bacterium Clostridium difficile (Clostridium Difficile Associated Diarrhea, CDAD), especially its Clostridium difficile NAP1/BI/02 strain, which is spreading rapidly in Europe and North America. This strain increases the frequency and severity of infections, requiring prompt diagnosis and treatment to prevent serious consequences. C. difficile accounts for about 20% of AAD cases and almost all cases of pseudomembranous colitis.
When to See a Doctor
Most cases of AAD are mild and do not require treatment, usually resolving a few days after stopping the antibiotics. However, in some cases, diarrhea can be more severe. Consult a doctor if you are taking antibiotics and notice:
- More than five episodes of loose stools a day.
- Severe, watery diarrhea.
- Fever.
- Abdominal pain or tenderness.
- Presence of pus or blood in the stool (if the disease progresses to colitis caused by C. difficile).
Sometimes fever and abdominal pain can occur a few days before the onset of diarrhea.
Prevention
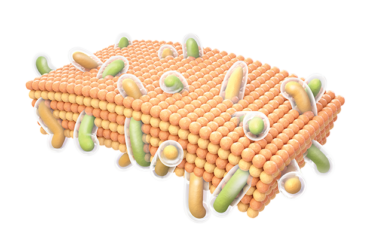
Key methods for combating AAD include early diagnosis, effective treatment, and controlling the spread of infection. Probiotics play an important role in protecting and restoring gut microbiota while taking antibiotics, as they:
- Strengthen the gut barrier.
- Improve immune response.
- Help prevent complications.
Studies have shown that adding symbiotic probiotic blends (S. thermophilus, B. longum, B. bifidum, L. acidophilus, and L. rhamnosus) to a two-week course of antibiotics during the eradication of Helicobacter pylori significantly reduced diarrhea frequency by 84.2%, confirming their high efficacy.
Thus, the combined use of probiotics with antibiotics helps reduce the risk of developing antibiotic-associated diarrhea and facilitates patient recovery.
Recommendations
- Do not take antibiotics on your own. Medication should be prescribed by a doctor based on appropriate laboratory analysis.
- Follow the prescribed dosage and do not change the treatment course without consulting a doctor.
- Inform your doctor of any side effects, including diarrhea, after starting antibiotic therapy.
Careful attention to symptoms and adherence to recommendations will help prevent serious consequences of antibiotic therapy.
Source: Mayo Clinic